Emergency rooms confront ‘tidal wave of sadness’ among young patients

GRAND RAPIDS—By the time Dr. Matthew Denenberg began a recent shift, his colleagues in the pediatric emergency department at Helen DeVos Children’s Hospital had already treated a day’s worth of illness and falls.
Child mental illness during COVID-19 (Second of three parts)
- Wednesday: The strain on families
- Today: Bureaucracy but no beds
- Friday: Fixing a threadbare system
There were ear aches and respiratory ailments along with a broken leg, a broken arm, injuries from an ATV accident and a bicycle spill — the usual catalogue of childhood chaos.
The ER staff is used to mending bones, starting IVs, hooking up heart monitors and taking temps. But what’s changed dramatically in the past year or so since COVID is the volume of children and teens with acute depression or other behavioral emergencies.
These patients “are confused or having psychiatric issues and want to hurt staff,” Denenberg said. “We’ve had staff choked, doors kicked in, walls with holes in them.”
At least 10 children and teens were in some form of emotional crisis on this day in mid June. They were taken to rooms inside the children’s ER, with its soft green walls and whimsical animal prints. Or sent to the 10th floor. On days like this, the emergency department essentially serves as a holding station until beds can be found for the most troubled patients at psychiatric centers.
Related:
- A child mental-health fix takes early action, more help. Here are 7 ideas.
- Mental health crisis: Children at breaking point during COVID
- Mentally ill suspects get help in Miami, jail in Michigan. Guess which works
- Michigan nears 1 million COVID cases. These numbers define the pandemic.
As an infant wailed, one more teen was being admitted. He would soon join the others on the 10th floor, an area converted recently for the overflow. A security guard was assigned to a bank of monitors for each room in case patients tried to harm themselves or were in distress.

Such scenes have unfolded with increased frequency for years. But they are far more common since COVID. A shortage of child psychiatrists and therapists and not nearly enough inpatient beds mean ER nurses and doctors often find themselves doubling as guardians, minders and care coordinators — for days or even weeks at a time.
It’s a lose-lose proposition: Patients are kept comfortable and cared for, but receive little to no serious treatment. And ER staff, already battered by a year of pandemic, must divert considerable resources to keeping young patients safe as they search for a psychiatric facility or clinic to take them.
“We should never hold a child here for 24 hours, but there’s no place to put them in the state of Michigan,” said Alan Vierling, president of Sparrow Hospital in Lansing.
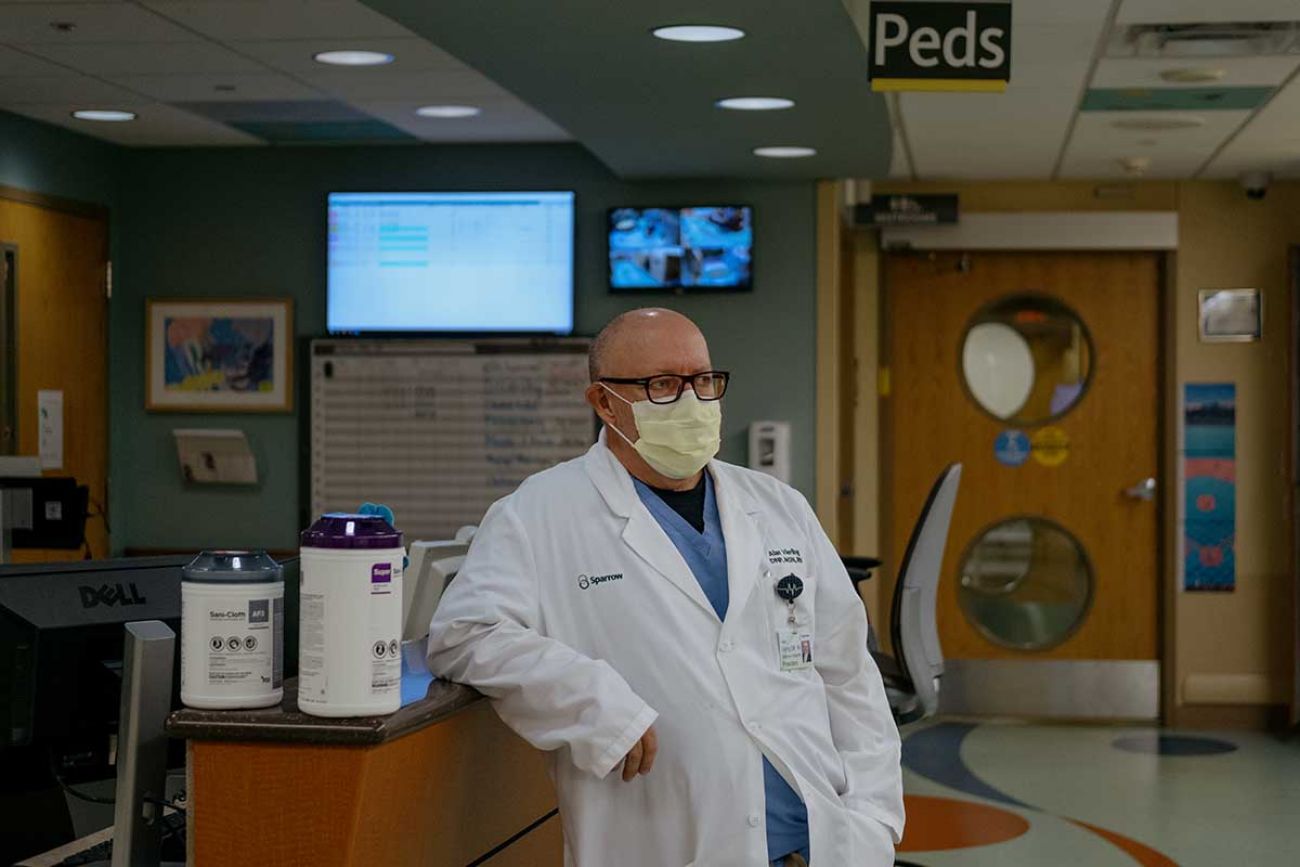
In a 40-year career that spans eight states, Vierling said he’s never seen such a “tidal wave of sadness,” a sentiment echoed by leaders in other Michigan health systems.
“I’ve seen a lot of sad things but I think this is the most difficult.”
In neighboring Indiana, hospital administrators say they’ve seen pediatric mental-health volumes shatter previous records. One hospital’s mental health assessment team says they worked with 1,200 adult and pediatric patients in a single month. Even in summer, when the hospital typically sees fewer pediatric cases, they’ve remained high.
One Indiana hospital said it has fielded calls from people several states away seeking an in-patient bed.
“You look at these kids — a beautiful six year old, a beautiful seven year old, a teenager who has got all of their future…” said Vierling of Sparrow. “And they’re in just desperate situations. It just breaks your heart.”
Finding a bed, getting past insurance
Adding to the logjam, some psychiatric inpatient facilities aren’t always eager to accept difficult cases. Insurance, or lack of it, often plays a role, sometimes in unexpected ways.
Kari Zoscsak, an ER nurse at Munson Healthcare Manistee Hospital, said she’s heard plenty of explanations for why an inpatient facility won’t take a youngster in crisis.
The kid’s too violent. Not at-risk enough. Too young. Too old. Been here too many times; we can’t help.
Cassandra Phipps, director of the Detroit Wayne Integrated Health Network’s children’s initiative, said some facilities have told her a youngster’s “mental health needs are too acute to address.’”

Health officials and some families said having good, employer-sponsored health insurance won’t guarantee quicker treatment, whether at their local hospital or an inpatient facility. In fact, private insurance can sometimes work against them.
Medicaid covers a wide array of behavioral health benefits, short- and long-term, and its beneficiaries often are able to tap into limited mental health resources in states like Michigan or Indiana more readily than those on employer-sponsored insurance that often covers only some services and for limited periods.
“If you don’t have Medicaid, nine out of 10 times you’re going to end up in the emergency room” rather than in treatment, said Jane Shank, executive director of the Lansing-based Association for Children’s Mental Health, which helps connect children with services.
And compared to other medical specialties, people are more likely to pay for mental health care out-of-pocket. Psychiatrists trained to work with children and adolescents are so few, they can demand high out-of-pocket fees without the limits of managed care.
“A lot of psychiatric providers don't accept insurance... they just don't want to deal with it,” said Holly Wheeler, director of Family Voices Indiana, which connects families with resources. “And frankly, they have the luxury of saying I don't want to deal with it.”
Dominick Pallone faced roadblocks when his second-grader began fighting with teachers, lashing out at home and trying to run away.
If anyone should know how to leverage insurance it’s Pallone. He’s executive director of the Michigan Association of Health Plans, which represents nearly every large Michigan insurer.
He said a therapist paid by his health insurer, Blue Cross Blue Shield of Michigan, suggested his family turn to a local, publicly-funded Community Mental Health agency for help getting his son intensive and comprehensive “wraparound” services not typically covered by Blue Cross. But the local CMH told Pallone it could only help if the child was covered by Medicaid.
“Most Michiganders think there’s this safety net thing called the Community Mental Health system, and so if I need help, regardless of the payer, I should be able to get it,” said Bob Sheehan, executive director of the Community Mental Health Association of Michigan. “It’s actually not true.”
Pallone said it took two years navigating through a thicket of providers and paperwork to get his son qualified for one of a limited number of Medicaid waivers set aside for children in a serious crisis.
“It's very taxing on families,” said Wheeler of Family Voices Indiana. “And if you don't have the means and the resources, then I guess you're out of luck.”
Give up your kid, get quicker care
Two Michigan families and one from Indiana told Bridge and Side Effects they were advised their kids could get more immediate psychiatric treatment if they relinquished parental rights to the state. Kevin Fischer, executive director of the Michigan chapter of the National Alliance on Mental Illness, said he frequently hears the same stories from families who contact him.
In February, one parent, Jay Gross of Mount Pleasant, posted a Facebook video from the parking lot of the MidMichigan Medical Center – Gratiot, in Alma. He’d just learned his 15-year-old son, who’d been suicidal, would be spending his 12th night at the hospital as staff sought to find inpatient treatment.
He didn’t blame the hospital, for which he had only praise. His fury was directed at the healthcare system.

“We’re told some of the most ridiculous things I’ve heard in my lifetime,” Gross said. “‘Your insurance is too good.’ ‘If (you) were to abandon him...it might speed up the process.’”
The video garnered more than 100,000 views and, a day later, his son was admitted to inpatient care.
Gross, a school teacher, recently told Bridge he’s still trying to get his head around the perversities of mental-health bureaucracy.
“I’m laughing and crying at the same time because of the insanity and the pain,” he said, as his son, who has since returned home, mowed the lawn on a blue-sky morning.
“That system isn’t just broken,” Gross said. “It’s disgusting.”
In Oakland County, north of Detroit, Sara and Nick Schmierer spent two years in emergency rooms and working with mental-health workers before making a heart-wrenching choice: signing over to the state an 8-year-old boy they’d taken in when he was abandoned as an infant.
The Schmierers, who became his legal guardians, were expecting their second set of twins when a stranger handed them the baby in a parking lot. They said the boy learned to crawl and play and giggle alongside the twins after their birth months later.
But as he neared his fifth birthday, he began to rage, throwing toys at walls and lashing out at siblings for little or no reason. And he began to have delusions.

The boy said he saw a snake on his father, or smelled fire that wasn’t there. One day, another son came downstairs to say his brother “wants to hurt himself. He doesn’t want to be here anymore,” Sarah Schmierer recalled.
She raced upstairs. There were monsters, the boy cried.
“All I could do was just hold on, like, ‘Buddy, I’m here. I love you...I know this is so scary for you. I don’t know what you’re thinking.’”
The boy turned and ran toward the window. “I grabbed him,” the mom said, and realized, “We need help, like this is more than I can do.”
He had just turned six.
“There is no facility ... that would take a child that young,” Sara Schmierer said. (The problem is worse since COVID. A Centers for Disease Control and Prevention study showed a 24 percent increase in mental health ER visits for very young children, ages 5 to 11, from April through October of last year.)
Thus began a two-year cycle of suicide attempts, ER trips, waits for beds, fights with insurers and school, and more violence. Nick Schmierer said he once grabbed a knife from his son’s hand as the boy tried to stab his sister. They got two German Shepherds to protect their other children.
At one point, they drove the boy to an Ohio facility after being told inpatient beds were full in Michigan.
Their journey is recorded in thick, three-ring binders the parents kept with insurance papers, admission forms and psychiatric assessments: reactive attachment disorder, disruptive mood dysregulation disorder, oppositional defiant disorder, ADHD, and more.
Finally, last fall, amid Michigan’s second wave of COVID, the boy erupted again. He was rushed to the ER and sedated. In a cell-phone video, he is seen thrashing in restraints, begging to be hugged. But when anyone approached, he bit or head butted them, the mother said.

For days, the boy remained in the hospital as staff sought an open bed at a psychiatric facility. Sarah Schmierer tried to soothe him with a calm voice and coloring books. He pleaded for a hug. She said, “Honey, I’m sorry, I can’t do that. You’re still trying to hurt me.”
She said he looked at her, without emotion, and said, “I’m going to kill you.”
With the afternoon sun streaming in her suburban Oakland County home recently, Schmierer said she never wanted to give up on her son. She was his mother.
Hear an Indiana mother’s fight to get her son services
But the violence. The bureaucratic fight to get help. The endless nights in ERs. That he returned home again and again no better than before. The couple said they also feared for the safety of their other kids.
So as the boy struggled in the ER last fall, they turned over guardianship to the state.
Their final image of the boy was of him trying to bite off his restraints as he was taken to the Hawthorn Center, a state-operated psychiatric hospital.
“Oh my gosh,” Sarah Schmierer thought to herself, “what have I done?”
A jump in attempted suicides
Bob Nykamp of Pine Rest Christian Mental Health Services, a sprawling Grand Rapid-based psychiatric center, recalls a lull early in the pandemic followed by an explosion of patients at its inpatient facilities.
At first, “families hunkered down. They didn't want to go to emergency rooms, because they were afraid of getting COVID. Volumes dropped,” Nykamp said
“That dip was like a month and a half, and then it just skyrocketed back up again.”
Inpatient admissions climbed 19 percent among young patients in 2020, according to Pine Rest, in part because the campus opened a 26-bed temporary unit for adolescents last year to accommodate overflow.
Other providers noted a similar pattern.
Across Michigan, more children on Medicaid or without insurance have been admitted each year for inpatient psychiatric services since 2016. But during the pandemic last year, statewide admissions actually went down — from 3,356 in 2019 to 3,091 in 2020.
Michigan officials speculate that the same COVID-related fears that kept people from visiting hospitals or doctors’ offices for other medical problems in 2020 tamped down, at least temporarily, psychiatric care as well.
Whatever the cause, inpatient psychiatric visits are now surging, with 1,944 before the end of June, according to the Michigan Department of Health and Human Services.

Nationally, the Centers for Disease Control and Prevention report that mental-health-related ER visits among adolescents aged 12 to 17 went up 31 percent in 2020. In a follow-up report this month, the agency said the pandemic has been particularly hard on young girls, with ER visits involving adolescent girls attempting suicide rising 51 percent early this year over the same period in 2019.
Parents notice the stress, too. Nearly 30 percent of parents of K-12 students said their children were "already experiencing harm" to their emotional or mental health because of social distancing and school closures, according to a Gallup poll of 1,232 parents taken in May.
Netflix and Goldfish crackers
None of this is news to the doctors, nurses and medical staff in hospital ERs, who have had to learn on the fly.
“There is no book that you can open up and read the guidelines and say this [is how] you’re going to take care of these kids with these special needs,” said JJ Brandt, a nurse in Sparrow’s pediatric ER.
“You really go in with, you know, an open mind, a big open heart and a lot of prayers.”
And sometimes you go in with Goldfish crackers, as Dr. Mark Hamed, director of the emergency and hospitalist departments at McKenzie Health System in Michigan’s Thumb region, did recently.
“We have a limited staff as it is,” Hamed said, explaining his quick stop at a Walmart before work to buy a boy’s favorite snack.

And so it goes. Nurses bring in coloring books. Dietary staff bring in favorite foods. Or they queue up Netflix. Anything, they said, to keep struggling kids calm and occupied as they wait for help.
But what hospital workers have been unable to do is relax. The stakes are too high, they say, their patients’ health too precarious.
Denenberg, the doctor at Helen DeVos, who is also vice president for medical affairs at Spectrum Health Grand Rapids, said the hospital has had to seek special medical masks for young patients in crisis. Some of the children were extracting the wire in conventional masks to cut themselves.
He has seen staff quit over the endless waits facing mentally ill children. And he understands their frustration. Nurses told him they didn’t “sign up to put a child in a room that was 14x14 and keep them there for seven days,” Denenberg said. “Imagine that.”
Coming Friday: Fixing the threadbare system
Suicide Prevention Help in Michigan
If you or someone you know is contemplating suicide, there are people who can help. Call the National Suicide Prevention Lifeline at 800-273-8255 (800-273-TALK) 24/7. The group also lists resources for anyone who may be contemplating suicide: www.suicidepreventionlifeline.org.
Some national and local resources are tailored to your needs — for youth, the LGBTQ+ community, Native Americans, Spanish speakers, military veterans, or those who are deaf or hard of hearing, for example.
Local providers can be found here through the U.S. Substance Abuse and Mental Health Services Administration. Crisis lines in Michigan also are searchable by county through the Michigan Department of Health and Human Services.
The state’s Michigan Warm Line — 888-PEER-753 (888-733-7753) — provides people with mental illness with emotional support from a certified peer support specialist or peer recovery coach every day from 10 a.m. to 2 a.m.
In Oakland County and the Upper Peninsula, residents may call the new Michigan Crisis and Access line at 844-44-MICAL (844-446-4225) or chat live through this webpage.
Loved ones should take action, and take seriously, if they notice someone:
- Talking about wanting to die
- Searching for ways to kill themselves, such as searching online or buying a gun
- Talking about feeling hopeless, having no reason to live, feeling trapped, being in unbearable pain or being a burden to others
- Increasing the use of alcohol or drugs
- Acting anxious or agitated; behaving recklessly
- Sleeping too little or too much
- Withdrawing or isolating themselves
- Showing rage or talking about seeking revenge
- Extreme mood swings
For more information about how to take action for someone else, check out these suggestions.
See what new members are saying about why they donated to Bridge Michigan:
- “In order for this information to be accurate and unbiased it must be underwritten by its readers, not by special interests.” - Larry S.
- “Not many other media sources report on the topics Bridge does.” - Susan B.
- “Your journalism is outstanding and rare these days.” - Mark S.
If you want to ensure the future of nonpartisan, nonprofit Michigan journalism, please become a member today. You, too, will be asked why you donated and maybe we'll feature your quote next time!








