Legal painkillers fuel spike in fatal ODs
On any given day, what’s worrying Michiganians about the illicit drug scene is likely to reflect what’s been in the news lately. When a Farmington Hills teenager allegedly beat his father to death with a baseball bat earlier this year, his lawyer blamed his use of synthetic marijuana. When a man in Miami attacked another and chewed on his face, the worries turned to so-called bath salts, the drug he was said to be using. (An investigation showed he was using marijuana.)
But year after year, the identifiable drugs that kill more state residents than any other are ones prescribed by doctors, widely taken for medical purposes, paid for by insurance and aren’t illicit at all – opioid pain relievers. You might know them by their brand names -- OxyContin. Vicodin, Opana, Percoset and others.
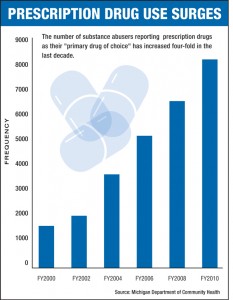
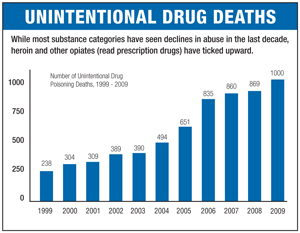
More Americans now die of drug overdoses than in auto accidents, and Michiganians are no different; in 2009, the last year for which comparative numbers are available, 871 state residents died in traffic fatalities, while 1,000 died of accidental overdose, according to the state’s Department of Community Health. What's more, a recent MLive analysis found that drug-related traffic accidents in the state are up 22 percent, with 26 deaths attributed to drugged driving last year. The trend is being driven by an explosion in legal prescriptions for the drugs, which are highly effective in treating chronic pain but also easily abused by patients and recreational users alike.
 Further, that trend is driving a spike in illegal drug use, particularly heroin, which is in the same chemical family as opioid pain relievers, but has the “advantage” – to the addict -- of being far less expensive. Last year, heroin was second only to alcohol as the self-reported drug of choice for residents seeking addiction treatment in publicly funded centers, according to MDCH data.
Further, that trend is driving a spike in illegal drug use, particularly heroin, which is in the same chemical family as opioid pain relievers, but has the “advantage” – to the addict -- of being far less expensive. Last year, heroin was second only to alcohol as the self-reported drug of choice for residents seeking addiction treatment in publicly funded centers, according to MDCH data.
Why is this happening? Because life hurts.
Pain treatment in the U.S. underwent a transformation at the end of the 20th century. Before the mid-’90s, powerful, opiate-based painkillers were used mainly in palliative care for those suffering pain from end-stage cancer, surgery or other short-term conditions. The risk of dependency and death was great enough that doctors were leery of letting too many such pills get into patient hands.
“When did it change? That’s easy,” said Dr. Andrew Kolodny, president of Physicians for Responsible Opioid Prescribing. “The real turning point was (in 1995), when Purdue Pharma introduced OxyContin.”
The tide had been turning for some years, with doctors beginning to believe that chronic pain was something to be treated rather than tolerated. But OxyContin represented a leap forward for pain treatment – it worked for 12 hours, relieving sufferers for longer periods of time. And it was aggressively marketed, with an “educational campaign focused on convincing doctors that opioids were under-utilized for non-cancer pain,” Kolodny said.
In 2007, the company would pay $634.5 million to 26 states and the District of Columbia, settling claims it misled doctors and patients alike about the drug’s abuse potential. Three Purdue Pharma executives pleaded guilty to criminal charges. But by then, the treatment philosophy they helped usher in – that powerful painkillers could be used to treat chronic conditions – had taken hold.
Doctors, Kolodny said, now have become too free with the prescription pad, writing “scrips” for 30 pills for a wisdom-tooth extraction “when two would do.”
State officials agree.
“Most prescribing physicians are not trained as pharmacologists,” said Larry Scott, manager of the prevention section at MDCH. “There's been some effort around the country to educate doctors, but we don't have a cadre of professionals coming out of those schools grounded in substance-abuse issues -- much less the pharmacology involved.”
Prescriptions for oxycodone (generic for OxyContin) rose 112.9 percent between 2003-2010, matched by similar rates for related drugs – Dilaudid (274.6 percent), methadone (146.1 percent) and Vicodin (85.3 percent). All can lead to dependence if used over the long term -- and dependence leads to addiction.
(Although the terms are sometimes used interchangeably, dependence and addiction are different concepts. Long-term use can lead to a physical dependence, meaning a person may suffer withdrawal symptoms if use is curtailed abruptly. Addiction refers to the compulsive use of an addictive substance, at the expense of the addict’s other daily activities.)
A complicated web of factors is feeding the problem, Scott said. An aging, overweight population suffers more pain, has more surgery and requires more drugs. And even with a burgeoning number of accidental overdoses, patients have come to believe that if they have chronic pain, they have a right to medicine to control it.
(Analysis of Michigan fatal overdose data/Michigan Department of Community Health)
Scott Masi, a recovering addict who now works in outreach and referral for Brighton Center for Recovery, a rehab hospital in Livingston County, sees the result every day of what he calls our drug-seeking society.
“We consume 99 percent of the world's hydrocodone and 90 percent of the world's opiates. Are we any different from any other society when it comes to pain?”
Masi said Brighton’s 18- to 25-year-old addict population is increasing, in part as a result of licit and illicit opioid use. In 1992, 10.5 percent of people in that age group were using injectable drugs; by 2009, that figure had risen to 26.9 percent.. Although marijuana is the most commonly used illicit drug by younger people, 8 percent reported having used Vicodin (hydrocodone) in the past year, according to the National Institutes of Health.
Opioids’ legal status complicates control efforts. Michigan House Rep. Lesia Liss, a former emergency-room nurse, said health-care workers are well aware of the habits of chronic abusers and doctor-shopping patients, but are limited in what they can do.
“We’d see a lot of patients coming in complaining of tooth pain,” she said. “We have no way of verifying it, and one of the questions we have to ask is for them to rate their pain on a scale of one to 10. And we have to accept their answer.”
Federal patient-privacy laws prohibited nurses from keeping lists of drug-seeking patients, although she said word would travel between hospitals on the worst offenders. Still, the problem never went away. Liss said more doctors need to take advantage of the Michigan Automated Prescription System, which allows health-care professionals to track patients’ prescription records of harder drugs.
“They can check, but it’s not a mandate,” said Liss, who co-sponsored a bill that became Public Act 44, allowing insurance companies and other benefits providers to access the system, as well.
Masi and others said the ready availability of opiates won’t be curbed until doctors and patients alike realize the extent of the problem. Doctors should prescribe more cautiously and dispense fewer pills, said Kolodny. And patients should take advantage of drug-disposal events or simply throw their unused painkillers away.
“People think because they’re prescribed by a doctor, they’re safe,” said Masi. “They’re not safe.”
Staff Writer Nancy Nall Derringer has been a writer, editor and teacher in Metro Detroit for seven years, and was a co-founder and editor of GrossePointeToday.com, an early experiment in hyperlocal journalism. Before that, she worked for 20 years in Fort Wayne, Indiana, where she won numerous state and national awards for her work as a columnist for The News-Sentinel.
See what new members are saying about why they donated to Bridge Michigan:
- “In order for this information to be accurate and unbiased it must be underwritten by its readers, not by special interests.” - Larry S.
- “Not many other media sources report on the topics Bridge does.” - Susan B.
- “Your journalism is outstanding and rare these days.” - Mark S.
If you want to ensure the future of nonpartisan, nonprofit Michigan journalism, please become a member today. You, too, will be asked why you donated and maybe we'll feature your quote next time!